What happens during duodenal switch surgery?
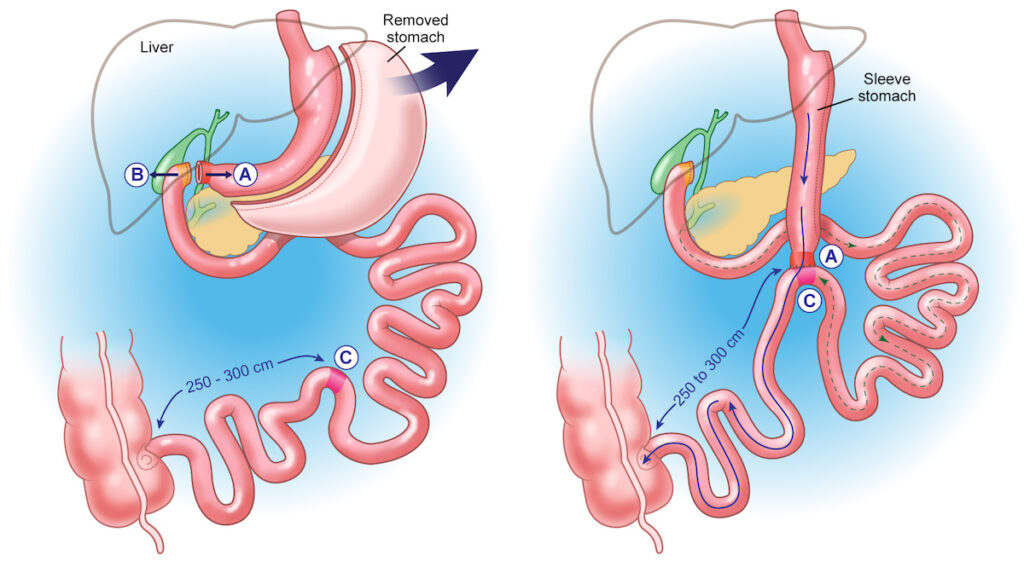
The ”switch”, or duodenal switch procedure in San Antonio, is a minimally invasive weight loss surgery combining features of the gastric sleeve and gastric bypass surgeries. Often called dual switch surgery or Duodenal Switch surgery, it’s performed in two primary stages:
- Gastric Sleeve: First, we remove approximately 80% of the stomach, creating a small, tube-like sleeve.
- Intestinal Bypass (“Switch”): Next, we bypass a significant length of the small intestine. Food travels directly from the gastric sleeve into the lower section of the small bowel, significantly reducing calorie and nutrient absorption.
At BMI of Texas, we specialize in a single-anastomosis or loop duodenal switch surgery, an advanced variation often called the modified duodenal switch (SADI-S). This modified approach simplifies traditional duodenal switch by requiring only one connection between the stomach and small intestine, reducing operative complexity and potential complications compared to traditional Duodenal Switch surgery.
“Of the four bariatric procedures we offer, this is the most drastic. As a result, it creates the most significant weight loss and offers the greatest chance of additional health benefits, such as remission of Type 2 diabetes and improved cholesterol.”
How much weight will I lose after duodenal switch surgery?
The duodenal switch bariatric surgery typically results in greater and more rapid weight loss compared to other weight loss procedures. When comparing duodenal switch vs gastric bypass, studies indicate that duodenal switch generally leads to significantly higher overall excess weight loss:
- 1-year average: 70-80% excess weight loss.
- 5-year average: 60-70% sustained excess weight loss.
- 10-year average: Approximately 60% long-term excess weight loss.
Additionally, this procedure significantly increases the chance of maintaining long-term weight reduction, improving insulin sensitivity, and providing better metabolic health outcomes.
Why should I consider loop duodenal switch surgery?
Generally, high-BMI (>50) diabetic patients are best suited for this procedure. However, it is widely known across all areas of modern medicine that obesity raises the risk of disease in nearly every system in the human body. Duodenal switch surgery can actively help reduce the risk and the effects of developing these diseases, including:
- Cardiovascular diseases: hypertension, arterial disease, vascular disease, heart attack, stroke
- Respiratory diseases: asthma, obstructive sleep apnea, obesity hypoventilation syndrome
- Metabolic diseases: hyperlipidemia, insulin resistance, and diabetes
- Gastrointestinal diseases: nonalcoholic fatty liver disease, nonalcoholic steatohepatitis
- Reproductive diseases: polycystic ovary syndrome, infertility
- Musculoskeletal pain: back strain, weight-bearing osteoarthritis
- Cancer: especially colorectal cancer and liver cancer
- Diabetes remission: Up to 90% of patients experience substantial improvement or complete remission of Type 2 diabetes.
Improved cholesterol and hypertension control: Patients commonly report significant improvements, reducing the risk of heart disease and stroke.
What are the dangers of duodenal switch surgery?
Like any other surgery, the Duodenal Switch procedure carries certain risks, which can include internal bleeding, infection, blood clots, and hernias. Risks associated with any abdominal surgery can also include excessive bleeding, adverse reactions to anesthesia, breathing problems, or leaks in your gastrointestinal system. You may also experience changes as your body reacts to rapid weight loss in the first three to six months, including body aches, flu-like symptoms, fatigue, dry skin, thinning hair, and mood changes. Longer-term risks and complications associated with Duodenal Switch surgery could include bowel obstruction, nausea or vomiting, diarrhea, gallstones, low blood sugar (hypoglycemia), malnutrition, stomach perforation, ulcers, bile reflux, diarrhea or frequent bowel movements, and, less likely, vomiting.
As is the case with all medical procedures, surgical complications can result in fatalities, and while extremely rare in occurrence, your medical condition and long-term history will be carefully assessed to mitigate all risk factors. But that’s only the beginning of our process to ensure your safe, successful, and long-lasting results. Our medical staff follows detailed pre- and post-surgical guidelines, which include rigorous candidacy assessments and multi-step precautions during surgery, as well as several in-person visits and careful monitoring of your weight loss experience once you leave our doors to begin your new, healthier life.

How long is the recovery from duodenal switch surgery?
Patients are usually kept in the hospital for one to three days following surgery, then a few weeks of additional recovery time at home. Your surgeon will want to see you for a follow-up visit two weeks after surgery, and then you will need to get onto a regular BMI of Texas follow-up schedule. During your recovery, your body will be going through huge changes, including rapid weight loss, and any severe symptoms should be reported to your BMI care team immediately.
You’ll also have very specific dietary guidelines during recovery, including not only what you can eat, but how you eat as well. These precautions are implemented to give your digestive system time to heal and adjust to its new digestive process. This transition phase typically takes one to two weeks and may primarily include liquids and soft foods as you return to your normal diet.
Thanks to advances in BMI’s Duodenal Switch surgical procedures, you will likely not experience dumping syndrome, which occurs when food, especially sugar, moves too quickly from the stomach to the duodenum. You will need to take additional regular daily vitamins (even more than other surgery patients) for the rest of your life. If you stop taking any prescribed vitamins, you will be more likely to develop a vitamin, mineral, or other nutritional deficiency.
To the average person, not getting enough vitamins may not sound like a big deal. However, when you “change the plumbing” with a duodenal switch, it can become a life-threatening problem. Nutritional complications with the duodenal switch include deficiencies in protein, iron, calcium, copper, zinc, and fat-soluble vitamins. You may be asked to eat differently if a protein deficiency is to occur.
Bowel movement changes are also more common with the Duodenal Switch than with other types of surgery. On average, Duodenal Switch patients will experience two to five bowel movements per day, but some patients have more. It is also not uncommon to have problems with diarrhea or loose stools, as well as foul-smelling stools or flatulence.
The board-certified team at BMI of Texas will prescribe supplements after surgery, such as:
- Multi-vitamin/mineral support
- Additional calcium
- Additional iron
- Fat-soluble vitamins (A,D, E, and K)
- Probiotics (beneficial bacteria found in the intestinal tract)
How do I begin?
If you want to learn more about San Antonio duodenal switch surgery, contact BMI of Texas at 210-405-6424.


